As in all animals, the adaptations for reproduction in humans are complex. They involve specialized and different anatomies in the two sexes, a hormone regulation system, and specialized behaviors regulated by the brain and endocrine system.
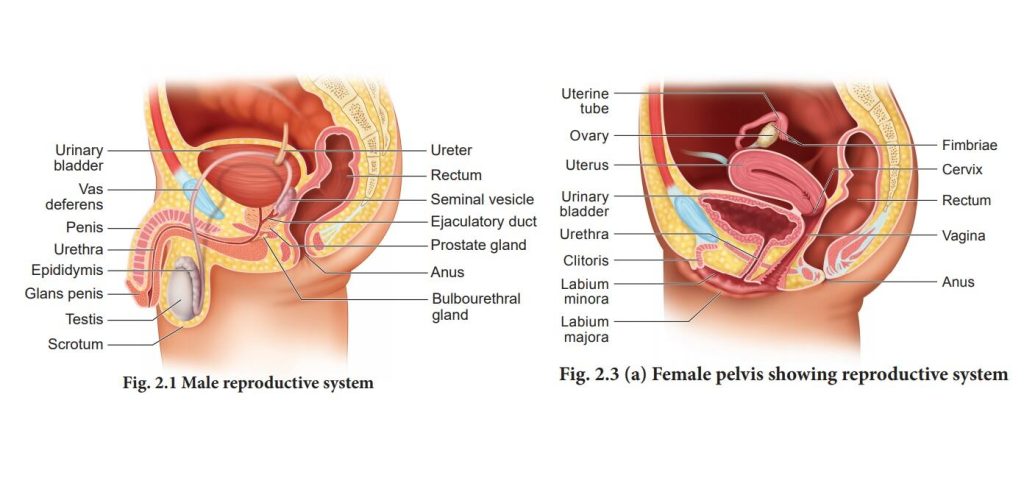
Human Reproductive Anatomy
The reproductive tissues of male and female humans develop similarly in utero until about the seventh week of gestation when a low level of the hormone testosterone is released from the gonads of the developing male. Testosterone causes the primitive gonads to differentiate into male sexual organs. When testosterone is absent, the primitive gonads develop into ovaries. Tissues that produce a penis in males produce a clitoris in females. The tissue that will become the scrotum in a male becomes the labia in a female. Thus the male and female anatomies arise from a divergence in the development of what were once common embryonic structures.
Male Reproductive Anatomy
Sperm are immobile at body temperature; therefore, the testes are external to the body so that a correct temperature is maintained for motility. In land mammals, including humans, the pair of testes must be suspended outside the body so the environment of the sperm is about 2 °C lower than body temperature to produce viable sperm. If the testes do not descend through the abdominal cavity during fetal development, the individual has reduced fertility.
The scrotum houses the testicles or testes (singular: testis), and provides passage for blood vessels, nerves, and muscles related to testicular function. The testes are a pair of male gonads that produce sperm and reproductive hormones. Each testis is approximately 2.5 by 3.8 cm (1.5 by 1 inch) in size and divided into wedge-shaped lobes by septa. Coiled in each wedge are seminiferous tubules that produce sperm.
The penis drains urine from the urinary bladder and is a copulatory organ during intercourse (Figure 13.12; Table 13.1). The penis contains three tubes of erectile tissue that become engorged with blood, making the penis erect, in preparation for intercourse. The organ is inserted into the vagina culminating with an ejaculation. During orgasm, the accessory organs and glands connected to the testes contract and empty the semen (containing sperm) into the urethra and the fluid is expelled from the body by muscular contractions causing ejaculation. After intercourse, the blood drains from the erectile tissue and the penis becomes flaccid.
Semen is a mixture of sperm (about five percent of the total) and fluids from accessory glands that contribute most of the semen’s volume. Sperm are haploid cells, consisting of a flagellum for motility, a neck that contains the cell’s energy-producing mitochondria, and a head that contains the genetic material (Figure 13.11). An acrosome (acrosomal vesicle) is found at the top of the head of the sperm. This structure contains enzymes that can digest the protective coverings that surround the egg and allow the sperm to fuse with the egg. An ejaculate will contain from two to five milliliters of fluid and from 50–120 million sperm per milliliter.
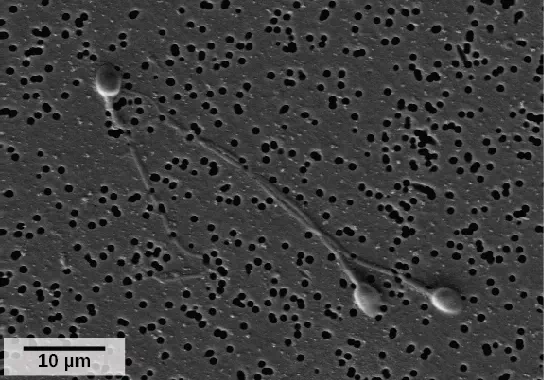
Figure 13.11 As seen in this scanning electron micrograph, human sperm has a flagellum, neck, and head. (credit: scale-bar data from Matt Russell)
Sperm form in the walls of seminiferous tubules that are coiled inside the testes (Figure 13.12; Table 13.1). The walls of the seminiferous tubules are made up of the developing sperm cells, with the least developed sperm at the periphery of the tubule and the fully developed sperm next to the lumen. The sperm cells are associated with Sertoli cells that nourish and promote the development of the sperm. Other cells present between the walls of the tubules are the interstitial cells of Leydig, which produce testosterone once the male reaches adolescence.
When the sperm have developed flagella they leave the seminiferous tubules and enter the epididymis (Figure 13.12; Table 13.1). This structure lies along the top and posterior of the testes and is the site of sperm maturation. The sperm leave the epididymis and enter the vas deferens, which carries the sperm behind the bladder, and forms the ejaculatory duct with the duct from the seminal vesicles. During a vasectomy, a section of the vas deferens is removed, preventing sperm (but not the secretions of the accessory glands) from being passed out of the body during ejaculation and preventing fertilization.
The bulk of the semen comes from the accessory glands associated with the male reproductive system. These are the seminal vesicles, the prostate gland, and the bulbourethral gland (Figure 13.12; Table 13.1). The secretions from the accessory glands provide important compounds for the sperm including nutrients, electrolytes, and pH buffering. There are also coagulation factors that affect sperm delivery and motility.
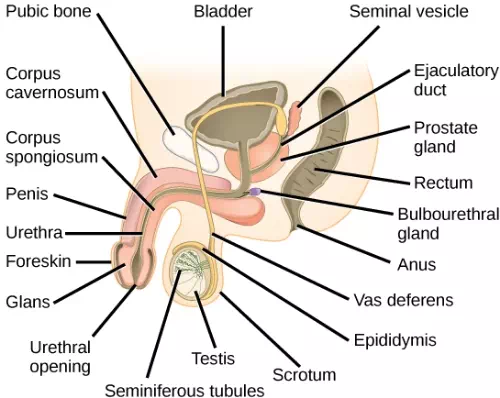
Figure 13.12 The reproductive structures of the human male are shown.
Which of the following statements about the male reproductive system is false?
A. The vas deferens carries sperm from the testes to the seminal vesicles.
B. The ejaculatory duct joins the urethra.
C. Both the prostate and the bulbourethral glands produce components of the semen.
D. The prostate gland is located in the testes.
<–D–>
| Table 13.1 Male Reproductive Anatomy | ||
| Organ | Location | Function |
| Scrotum | External | Supports testes and regulates their temperature |
| Penis | External | Delivers urine, copulating organ |
| Testes | Internal | Produce sperm and male hormones |
| Seminal Vesicles | Internal | Contribute to semen production |
| Prostate Gland | Internal | Contributes to semen production |
| Bulbourethtral Glands | Internal | Neutralize urine in urethra |
Female Reproductive Anatomy
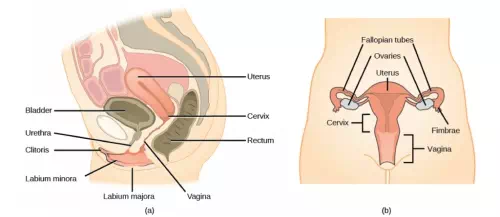
Figure 13.13 A number of female reproductive structures are exterior to the body. These include the breasts and the vulva, which consists of the mons pubis, clitoris, labia majora, labia minora, and the vestibular glands (Figure 13.13; Table 13.2).
The breasts consist of mammary glands and fat. Each gland consists of 15 to 25 lobes that have ducts that empty at the nipple and that supply the nursing child with nutrient- and antibody-rich milk to aid development and protect the child.
Internal female reproductive structures include ovaries, oviducts, the uterus, and the vagina (Figure 13.13; Table 13.2). The pair of ovaries is held in place in the abdominal cavity by a system of ligaments. The outermost layer of the ovary is made up of follicles, each consisting of one or more follicular cells that surround, nourish, and protect a single egg. During the menstrual period, a batch of follicular cells develops and prepares their eggs for release. At ovulation, one follicle ruptures and one egg is released. Following ovulation, the follicular tissue that surrounded the ovulated egg stays within the ovary and grows to form a solid mass called the corpus luteum. The corpus luteum secretes additional estrogen and the hormone progesterone that helps maintain the uterine lining during pregnancy. The ovaries also produce hormones, such as estrogen.
The oviducts, or fallopian tubes, extend from the uterus in the lower abdominal cavity to the ovaries, but they are not in contact with the ovaries. The lateral ends of the oviducts flare out into a trumpet-like structure and have a fringe of finger-like projections called fimbrae. When an egg is released at ovulation, the fimbrae help the nonmotile egg enter into the tube. The walls of the oviducts have a ciliated epithelium over smooth muscle. The cilia beat, and the smooth muscle contracts, moving the egg toward the uterus. Fertilization usually takes place within the oviduct and the developing embryo is moved toward the uterus. It usually takes the egg or embryo a week to travel through the oviduct.
Sterilization in women is called a tubal ligation; it is analogous to a vasectomy in males in that the oviducts are severed and sealed, preventing sperm from reaching the egg.
The uterus is a structure about the size of a woman’s fist. The uterus has a thick muscular wall and is lined with an endometrium rich in blood vessels and mucus glands that develop and thicken during the female cycle. Thickening of the endometrium prepares the uterus to receive the fertilized egg or zygote, which will then implant itself in the endometrium. The uterus supports the developing embryo and fetus during gestation. Contractions of the smooth muscle in the uterus aid in forcing the baby through the vagina during labor. If fertilization does not occur, a portion of the lining of the uterus sloughs off during each menstrual period. The endometrium builds up again in preparation for implantation. Part of the uterus, called the cervix, protrudes into the top of the vagina.
The vagina is a muscular tube that serves several purposes. It allows menstrual flow to leave the body. It is the receptacle for the penis during intercourse and the pathway for the delivery of offspring.
| Table 13.2 Female Reproductive Anatomy | ||
| Organ | Location | Function |
| Clitoris | External | Sensory organ |
| Mons pubis | External | Fatty area overlying pubic bone |
| Labia majora | External | Covers labia minora; contains sweat and sebaceous glands |
| Labia minora | External | Covers vestibule |
| Greater vestibular glands | External | Secrete mucus; lubricate vagina |
| Breast | External | Produces and delivers milk |
| Ovaries | Internal | Produce and develop eggs |
| Oviducts | Internal | Transport egg to uterus; site of fertilization |
| Uterus | Internal | Supports developing embryo |
| Vagina | Internal | Common tube for intercourse, birth canal, passing menstrual flow |