Hormones have a wide range of effects and modulate many different body processes. The key regulatory processes that will be examined here are those affecting the excretory system, the reproductive system, metabolism, blood calcium concentrations, growth, and the stress response.
Hormonal Regulation of the Excretory System
Maintaining a proper water balance in the body is important to avoid dehydration or over-hydration (hyponatremia). The water concentration of the body is monitored by osmoreceptors in the hypothalamus, which detect the concentration of electrolytes in the extracellular fluid. The concentration of electrolytes in the blood rises when there is water loss caused by excessive perspiration, inadequate water intake, or low blood volume due to blood loss. An increase in blood electrolyte levels results in a neuronal signal being sent from the osmoreceptors in hypothalamic nuclei. The pituitary gland has two components: anterior and posterior. The anterior pituitary is composed of glandular cells that secrete protein hormones. The posterior pituitary is an extension of the hypothalamus. It is composed largely of neurons that are continuous with the hypothalamus.
The hypothalamus produces a polypeptide hormone known as antidiuretic hormone (ADH), which is transported to and released from the posterior pituitary gland. The principal action of ADH is to regulate the amount of water excreted by the kidneys. As ADH (which is also known as vasopressin) causes direct water reabsorption from the kidney tubules, salts and wastes are concentrated in what will eventually be excreted as urine. The hypothalamus controls the mechanisms of ADH secretion, either by regulating blood volume or the concentration of water in the blood. Dehydration or physiological stress can cause an increase of osmolarity above 300 mOsm/L, which in turn, raises ADH secretion and water will be retained, causing an increase in blood pressure. ADH travels in the bloodstream to the kidneys. Once at the kidneys, ADH changes the kidneys to become more permeable to water by temporarily inserting water channels, aquaporins, into the kidney tubules. Water moves out of the kidney tubules through the aquaporins, reducing urine volume. The water is reabsorbed into the capillaries lowering blood osmolarity back toward normal. As blood osmolarity decreases, a negative feedback mechanism reduces osmoreceptor activity in the hypothalamus, and ADH secretion is reduced. ADH release can be reduced by certain substances, including alcohol, which can cause increased urine production and dehydration.
Chronic underproduction of ADH or a mutation in the ADH receptor results in diabetes insipidus. If the posterior pituitary does not release enough ADH, water cannot be retained by the kidneys and is lost as urine. This causes increased thirst, but water taken in is lost again and must be continually consumed. If the condition is not severe, dehydration may not occur, but severe cases can lead to electrolyte imbalances due to dehydration.
Another hormone responsible for maintaining electrolyte concentrations in extracellular fluids is aldosterone, a steroid hormone that is produced by the adrenal cortex. In contrast to ADH, which promotes the reabsorption of water to maintain proper water balance, aldosterone maintains proper water balance by enhancing Na+ reabsorption and K+ secretion from extracellular fluid of the cells in kidney tubules. Because it is produced in the cortex of the adrenal gland and affects the concentrations of minerals Na+ and K+, aldosterone is referred to as a mineralocorticoid, a corticosteroid that affects ion and water balance. Aldosterone release is stimulated by a decrease in blood sodium levels, blood volume, or blood pressure, or an increase in blood potassium levels. It also prevents the loss of Na+ from sweat, saliva, and gastric juice. The reabsorption of Na+ also results in the osmotic reabsorption of water, which alters blood volume and blood pressure.
Aldosterone production can be stimulated by low blood pressure, which triggers a sequence of chemical release, as illustrated in Figure 18.7. When blood pressure drops, the renin-angiotensin-aldosterone system (RAAS) is activated. Cells in the juxtaglomerular apparatus, which regulates the functions of the nephrons of the kidney, detect this and release renin. Renin, an enzyme, circulates in the blood and reacts with a plasma protein produced by the liver called angiotensinogen. When angiotensinogen is cleaved by renin, it produces angiotensin I, which is then converted into angiotensin II in the lungs. Angiotensin II functions as a hormone and then causes the release of the hormone aldosterone by the adrenal cortex, resulting in increased Na+reabsorption, water retention, and an increase in blood pressure. Angiotensin II in addition to being a potent vasoconstrictor also causes an increase in ADH and increased thirst, both of which help to raise blood pressure.
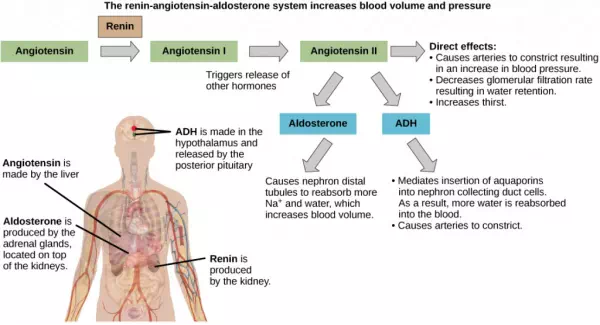
Figure 18.7.
ADH and aldosterone increase blood pressure and volume. Angiotensin II stimulates release of these hormones. Angiotensin II, in turn, is formed when renin cleaves angiotensin. (credit: modification of work by Mikael Häggström)
Hormonal Regulation of the Reproductive System
Regulation of the reproductive system is a process that requires the action of hormones from the pituitary gland, the adrenal cortex, and the gonads. During puberty in both males and females, the hypothalamus produces gonadotropin-releasing hormone (GnRH), which stimulates the production and release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary gland. These hormones regulate the gonads (testes in males and ovaries in females) and therefore are called gonadotropins. In both males and females, FSH stimulates gamete production and LH stimulates production of hormones by the gonads. An increase in gonad hormone levels inhibits GnRH production through a negative feedback loop.
Regulation of the Male Reproductive System
In males, FSH stimulates the maturation of sperm cells. FSH production is inhibited by the hormone inhibin, which is released by the testes. LH stimulates production of the sex hormones (androgens) by the interstitial cells of the testes and therefore is also called interstitial cell-stimulating hormone.
The most widely known androgen in males is testosterone. Testosterone promotes the production of sperm and masculine characteristics. The adrenal cortex also produces small amounts of testosterone precursor, although the role of this additional hormone production is not fully understood.
The Dangers of Synthetic Hormones

Figure 18.8. Professional baseball player Jason Giambi publically admitted to, and apologized for, his use of anabolic steroids supplied by a trainer. (credit: Bryce Edwards)
Some athletes attempt to boost their performance by using artificial hormones that enhance muscle performance. Anabolic steroids, a form of the male sex hormone testosterone, are one of the most widely known performance-enhancing drugs. Steroids are used to help build muscle mass. Other hormones that are used to enhance athletic performance include erythropoietin, which triggers the production of red blood cells, and human growth hormone, which can help in building muscle mass. Most performance enhancing drugs are illegal for non-medical purposes. They are also banned by national and international governing bodies including the International Olympic Committee, the U.S. Olympic Committee, the National Collegiate Athletic Association, the Major League Baseball, and the National Football League.
The side effects of synthetic hormones are often significant and non-reversible, and in some cases, fatal. Androgens produce several complications such as liver dysfunctions and liver tumors, prostate gland enlargement, difficulty urinating, premature closure of epiphyseal cartilages, testicular atrophy, infertility, and immune system depression. The physiological strain caused by these substances is often greater than what the body can handle, leading to unpredictable and dangerous effects and linking their use to heart attacks, strokes, and impaired cardiac function.
Regulation of the Female Reproductive System
In females, FSH stimulates development of egg cells, called ova, which develop in structures called follicles. Follicle cells produce the hormone inhibin, which inhibits FSH production. LH also plays a role in the development of ova, induction of ovulation, and stimulation of estradiol and progesterone production by the ovaries, as illustrated in Figure 18.9. Estradiol and progesterone are steroid hormones that prepare the body for pregnancy. Estradiol produces secondary sex characteristics in females, while both estradiol and progesterone regulate the menstrual cycle.
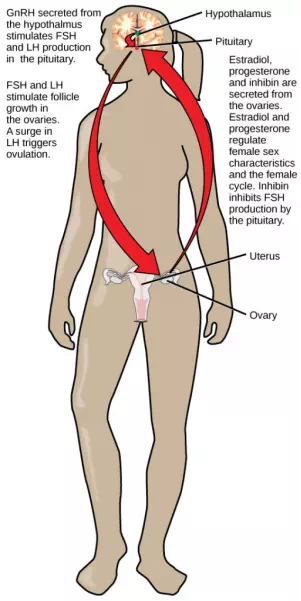
Figure 18.9. Hormonal regulation of the female reproductive system involves hormones from the hypothalamus, pituitary, and ovaries.
In addition to producing FSH and LH, the anterior portion of the pituitary gland also produces the hormone prolactin (PRL) in females. Prolactin stimulates the production of milk by the mammary glands following childbirth. Prolactin levels are regulated by the hypothalamic hormones prolactin-releasing hormone (PRH) and prolactin-inhibiting hormone (PIH), which is now known to be dopamine. PRH stimulates the release of prolactin and PIH inhibits it.
The posterior pituitary releases the hormone oxytocin, which stimulates uterine contractions during childbirth. The uterine smooth muscles are not very sensitive to oxytocin until late in pregnancy when the number of oxytocin receptors in the uterus peaks. Stretching of tissues in the uterus and cervix stimulates oxytocin release during childbirth. Contractions increase in intensity as blood levels of oxytocin rise via a positive feedback mechanism until the birth is complete. Oxytocin also stimulates the contraction of myoepithelial cells around the milk-producing mammary glands. As these cells contract, milk is forced from the secretory alveoli into milk ducts and is ejected from the breasts in milk ejection (“let-down”) reflex. Oxytocin release is stimulated by the suckling of an infant, which triggers the synthesis of oxytocin in the hypothalamus and its release into circulation at the posterior pituitary.