Tumor immunology refers to the relationship between immune function and tumor cells, which is crucial for our understanding of the mechanisms of both tumor rejection and tumor progression. The immunological mechanisms involved in cancer growth are highly complex, including tissue-resident and blood-derived cells. The human immune system mounts natural endogenous response to highly immunogenic tumor cells through a series of steps, including the presenting of tumor antigens to T cells via antigen-presenting cells (APCs), priming and activation of T cells in the lymph nodes, trafficking and infiltration of T cells into tumor beds, recognition of cancer cells by T cells, development of antigen-specific effector and memory T cells, and humoral immunity, allowing effector T cells and other endogenous immune cells, as well as tumor-effective antibodies to tumor to eliminate cancer cells.
Innate Immune Response to Tumor Cells
Cancer cells can alter the steady-state activity of all myeloid cells present in the tumor microenvironment by secreting factors such as interleukin (IL)-6 or granulocyte-macrophage colony-stimulating factor (GM-CSF), that induce the recruitment of immature myeloid cells to tumor cells, as well as cell proliferation.
Natural killer (NK) cells can kill target cells without the need for prior activation, especially in conditions that major histocompatibility complex (MHC) class I molecules (which at normal levels inhibit NK cells) are absent or under expressed in target cells. As many neoplastic cells lose the expression of MHC-I during malignant transformation, they continue to express ligands (e.g. glycolipid) that activate NK cells. This recognition mechanism further leads to the progression of antitumor immune response through the production of interferon-γ (IFN-γ). IFN-γ can activate a number of IFN-γ dependent signaling pathways which enhance the killing of a proportion of the tumor.
In addition, IFN-γ, released at a tumor site, induces the production of chemokines that further recruit more cells of the innate immune system to the tumor. Macrophages are recruited into tumors following activation of colony-stimulating factor 1 receptor (CSF1R) by either CSF1 or IL-34. Besides, the chemokine CCL2 may also facilitate the recruitment of macrophage. IFN-γ activates macrophages that express reactive oxygen and nitrogen metabolites which are tumoricidal products. Macrophage can also secret tumor necrosis factor (TNF) that activates endothelial cells and causes coagulation, leading to tumor necrosis and directly stimulating apoptosis. Moreover, cytokines such as IL-12, IL-15, and the type I interferons stimulate NK cells, which leads to proliferation and increased cytotoxic activity.

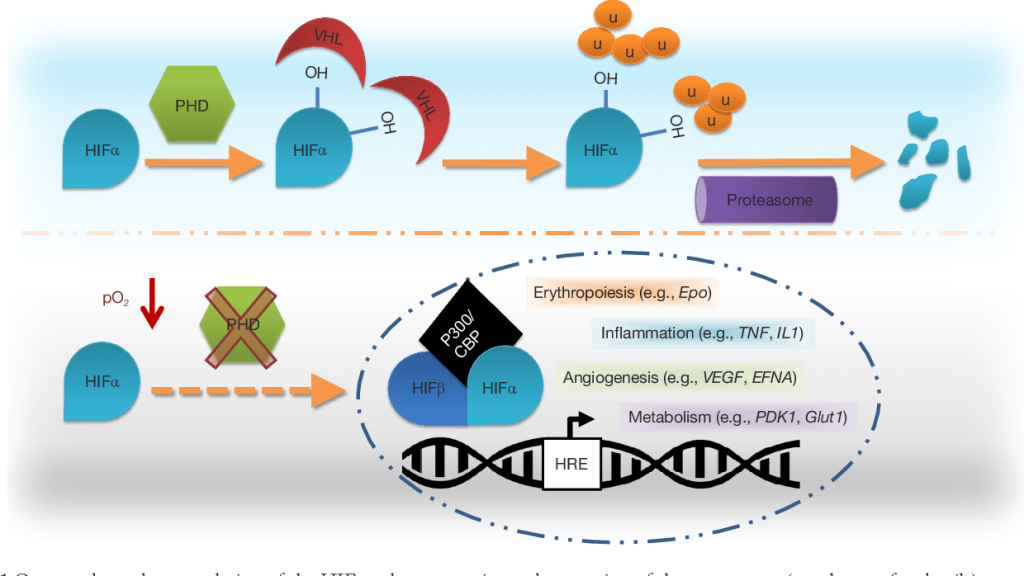
Figure 1. A model of innate and adaptive immunity to cancer cells. (De Visser KE et al., 2006)
Adaptive Immune Response to Tumor Cells
Cytotoxic T lymphocytes (CTLs) are the primary mechanism of tumor cell killing in adaptive immune response, which, in many cases, requires the participation of APCs to present the relevant tumor antigen to the CTLs in the appropriate conditions for an antigen-specific immune response. MHC-I and -II molecules must be present to stimulate the production of CTLs. Typically, MHC-I APCs, such as dendritic cells (DC), present antigen (tumor-derived peptides) to CD8+ T cells in the context of co-stimulation through CD80, CD70, and 4-1BB, as well as through DC-derived cytokines such as IL-12, type I interferon, and IL-15. CD8+ CTLs have been demonstrated in numerous different types of solid tumors in vivo and have been shown to cause tumor cell destruction in vitro.
CD4+ T helper cells release cytokines, leading to the anti-tumor immune reaction. The Th1-polarized CD4+ T cells secrete IL-2, TNF-α, and IFN-γ, which promote the development of CD8+ CTLs and the activation of macrophage cytotoxic activity. In addition, they can upregulate antigen processing and the expression of MHC-I and -II molecules in professional APCs such as macrophages and DCs. In contrast, Th2 polarized CD4+ T cells release cytokines IL-4, -5, -6, -10, and -13, resulting in T-cell anergy and loss of T-cell-mediated cytotoxicity, enhance humoral immunity, and regulate the tumor-promoting activities of macrophages.
In addition to the effector mechanism mediated by CTLs, the host immune system can generate specific antibodies against cancer antigens, which exert cytotoxic effect against the antigen-bearing tumor cells. Rather than recognizing only protein-derived antigens by T cell antigen receptors, antibodies can bind to multiple types of tumor antigens including polysaccharides, lipids, and proteins. This enhances the anti-tumor ability of the host immune system by broadening the number of tumor antigens that can be exploited for cytotoxic reactions. Mechanisms of antibodies mediated tumor cytotoxicity include antibody-dependent cell-mediated cytotoxicity and complement-mediated cytotoxicity.


Comments are closed